AI medical scribe: Top tools, benefits, and future outlook
Discover the future of healthcare with AI medical scribe: how they work, key benefits, top 5 tools shaping the market, and what’s next.
Doctors juggle patient care and mountains of documentation daily—so much so that nearly two hours of clinical time translates to hours of charting afterwards. But things are starting to shift. AI medical scribes are breaking into clinics and doctor’s offices, changing the way doctors handle clinical documentation.
Instead of forcing clinicians to split their attention with typing, these tools quietly listen during consultations, using speech recognition and NLP to capture key details. The result? Bright, context-aware notes that populate the electronic health record (EHR) automatically, so doctors can stay focused on the patient—not the keyboard. This translates into higher efficiency, reduced burnout costs, and stronger patient outcomes for organizations.
In this article, we’ll explore:
- How AI scribes actually work behind the scenes
- The most significant benefits they bring to doctors and healthcare providers
- The top 5 leading platforms in AI-powered clinical documentation right now
- What the future of AI scribes could mean for healthcare organizations
I. How does an AI medical scribe work?
An AI medical scribe uses speech recognition and natural language processing (NLP) to listen to the entire conversation and convert it into clear, structured clinical notes. Instead of typing everything by hand, doctors can rely on the tool to pull out the most important details—symptoms, diagnoses, prescriptions, and treatment steps—and place them directly into the electronic health record (EHR).
Here’s what the process usually looks like:
- Audio capture: records the doctor–patient conversation in real time.
- Speech-to-text: converts the audio into written notes with advanced voice recognition.
- NLP analysis: interprets context, medical terms, and key information.
- Information extraction: organizes data such as symptoms, diagnoses, and treatment plans.
- EHR entry: fills the right sections of the patient’s record automatically.
- Summary generation: provides a sharp, easy-to-read recap of the visit.
- Review: the doctor makes final edits and confirms the document.
The real value of an AI scribe lies in how much time it saves. Documentation is one of the most draining parts of a doctor’s day, and automating it frees up hours that would otherwise be spent on paperwork. With less admin work, doctors can focus on patients, make quicker clinical decisions, and build stronger connections during consultations. The result is better care for patients and less burnout for medical teams.
II. What are the benefits of AI medical scribes?
Although AI has entered many industries, healthcare has been slower to adopt. Surveys back this up: the RACGP reports that 83% of general practitioners rarely or never use AI, and research from Avant shows that only about 11% of doctors currently use AI scribes.
But those figures only reveal part of the story. In practice, AI medical scribes offer clear, everyday benefits that go beyond efficiency—they can actually improve both the patient and doctor experience:
- Less paperwork, more work-life balance
- Better quality consultations, thanks to more focus on the patient
- Accurate, detailed medical records with fewer mistakes
1. Reduced admin and a healthier work-life balance
One key benefit is having far less paperwork to deal with. Instead of spending hours at the end of a shift catching up on notes, doctors can let the system handle it. That translates to fewer late nights at the clinic, less weekend “catch-up work,” and more time at home with family.
2. Enhanced patient care
AI scribes also allow doctors to be fully present in the room. Without the distraction of typing, they can keep eye contact, listen carefully, and engage in a natural conversation.
In fact, the change is easy to spot. In a U.S. pilot with more than 10,000 doctors, patients mentioned how their doctors were “finally listening instead of just typing.” And in Australia, the Health of the Nation 2024 report pointed out that AI scribes lifted the quality of consultations and brought some of the enjoyment back into the job for many doctors.
Ready to Outsource?
Get top-tier IT talent without the hassle. Contact us now!
3. More accurate, detailed documentation
Accuracy is another big win. Because the scribe listens to the entire consultation and pulls out key details, the resulting documentation is often more precise and less prone to errors.
Take VoiceBox Scribe, for example. With just one recording, it can generate documents—from internal notes to patient-facing reports—without copying and pasting. Doctors who use it say they’ve even started speaking more clearly during consultations, knowing everything will be captured. That extra clarity doesn’t just improve the medical record—it also helps patients better understand their own health.
As AI medical scribes gain traction globally, explore Vietnam’s Top 10 AI Companies in Healthcare to watch in 2026 to discover innovators advancing AI-powered clinical documentation and intelligent healthcare automation.
III. Top 4 best AI-powered Clinical Documentation
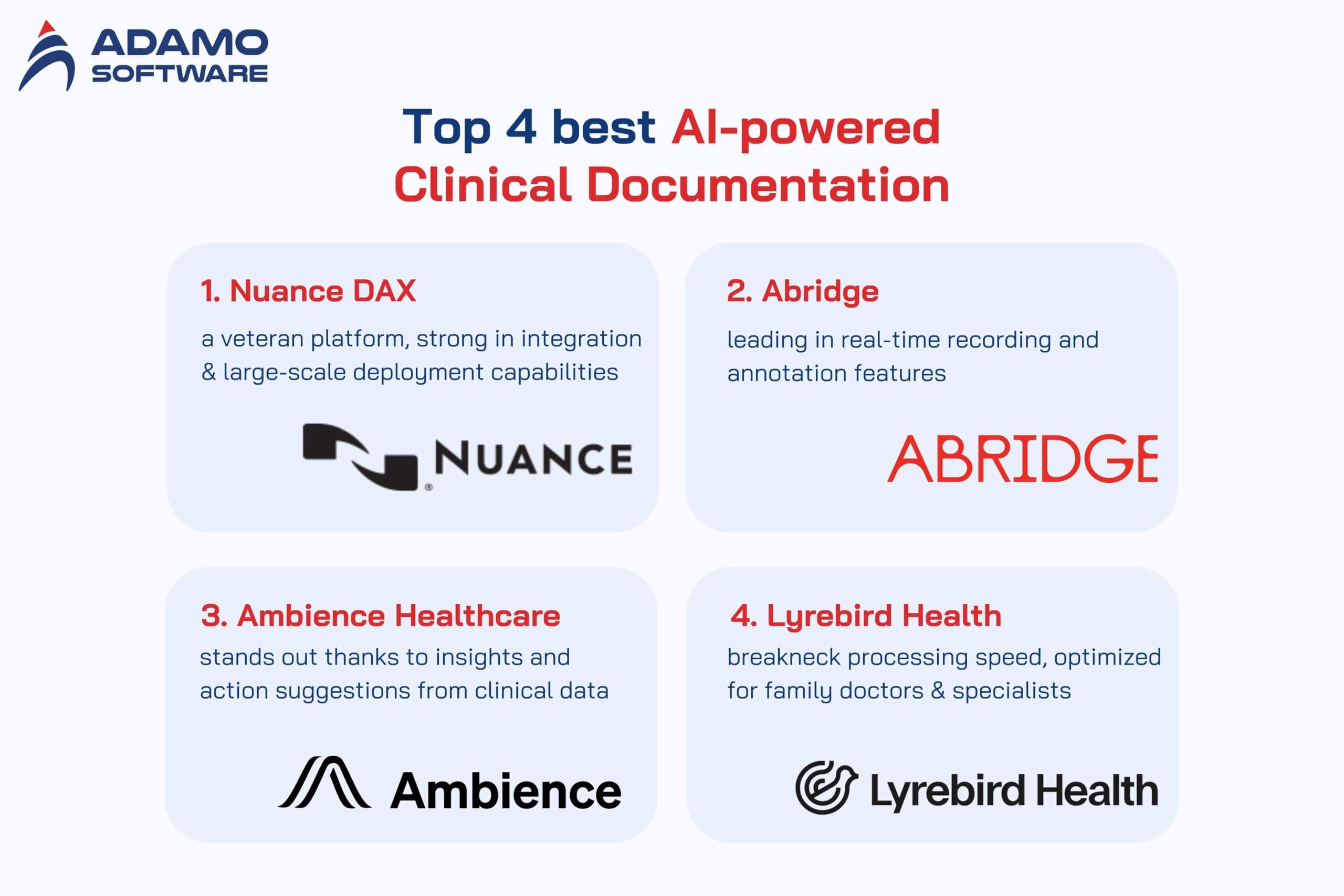
The AI medical scribe market is quite vibrant, with many different solutions from medical technology companies. Each platform has strengths, from transcription speed to EHR integration or accuracy. If you are considering choosing, here are the five most prominent names today:
- Nuance DAX: a veteran platform, strong in integration and large-scale deployment capabilities
- Abridge: leading in real-time recording and annotation features
- Ambience Healthcare: stands out thanks to insights and action suggestions from clinical data.
- Lyrebird Health: breakneck processing speed, optimized for family doctors and specialists
1. Nuance DAX
If there’s a “classic” in this space, it’s Nuance DAX. Backed by Microsoft, the platform has been around long enough to prove it can handle the demands of large hospitals. Its biggest strength? Offers seamless connections to major EHR platforms, including Epic and Cerner.
Doctors using DAX don’t need to worry about typing or formatting — they talk with their patients, and the system generates clean, standardized notes ready for approval. The experience feels smooth for both sides: less screen time for doctors, more face time for patients.
Key features:
- AI voice-enabled ACI
- Complete, standardized notes
- Good experience for both doctors and patients
- Top EHR integration
- Reference price: ~20,000 USD/year/doctor, no free trial
2. Abridged
While DAX represents stability and scale, Abridge shows what a nimble startup can do when it focuses on speed. This San Francisco–based platform has made a name for itself with real-time note-taking that works. Its ambient AI captures conversations as they happen so doctors can keep the flow natural.
Many doctors like Abridge because it integrates tightly with Epic and saves them dozens of hours each month. Imagine wrapping up your day without facing a mountain of unfinished notes — that’s the appeal here.
Key features:
- Real-time transcription
- Ambient AI hands-free
- Deep integration with Epic
- Automatic note generation in standard format
- Used by 10,000+ doctors
- Reference price: 2,500 USD/year/doctor, no free trial
3. Ambience Healthcare
Ambience takes a slightly different route. Beyond converting speech into text, it analyzes the conversation and surfaces insights. Think of it as an intelligent assistant that doesn’t just transcribe but also highlights what might matter for the next steps in care.
It works across devices — phone, tablet, even smart speakers — and connects to most big EHR systems. Ambiance offers both in one package for doctors who want documentation plus decision support.
Key features:
- Ambient voice intelligence platform
- Extract natural conversations into clinical data.
- Suggest actions and insights.
- Multiple EHR integrations
- Custom workflow & templates
- Reference price: 3,200 USD/year/doctor, no free trial
4. Lyrebird Health
For family doctors and specialists juggling back-to-back patients, speed is everything. What makes Lyrebird shine is its ability to generate reliable notes almost instantly — usually under 10 seconds. It’s especially popular in Australia, where it connects directly to Best Practice Software — a system many clinics already use.
Besides notes, it can also generate referral letters, prescriptions, and medical certificates in standard formats. That means fewer repetitive tasks and less time fiddling with documents.
Key features:
- AI ambient scribe & medical dictation
- High accuracy, lightning speed
- Simple, easy-to-use interface
- Pre-generate letters, reports, prescriptions, and treatment plans
- Personalized templates & community sharing
- Reference price: $2,400/year/doctor, 14-day free trial
IV. What to look forward to from AI Clinical Scribe in the future
AI scribes are no longer just a pilot project — they’re slowly becoming part of daily practice in many clinics. With the current wave of investment, it’s almost certain we’ll see more tools emerge, moving beyond simple note-taking. In the near future, doctors could expect features like automated follow-up reminders or even draft treatment plans tailored to each patient.
However, to reach that stage, deeper integration with EHRs is essential. AI can offer personalized suggestions only by sitting inside the medical record system. Of course, that raises a critical concern: how safe is patient data? Without strict safeguards and transparent mechanisms, sensitive information could be at risk.
Accuracy remains another roadblock. Studies show that AI-generated notes still require manual edits in most cases. Some even “hallucinate” details that never came up in consultation — a risk no doctor can afford. Human review remains the final safety net: AI can handle the heavy lifting, but doctors or scribes still hold the pen regarding accuracy.
There’s also the policy challenge. A few guidelines have been published, but they lag behind the speed of innovation. As adoption grows, healthcare leaders must balance two priorities: encourage new technology while ensuring patient safety.
In short, the potential is enormous. However, unlocking that potential will take balance: smarter tech, stronger safeguards, and the human touch AI can’t replace.
V. Final thoughts

AI medical scribes are quickly becoming an essential part of clinical workflows. Their impact is clear by reducing paperwork, improving the quality of consultations, and reducing administrative stress. For example, a recent report from the American Medical Association shows that AI scribes helped doctors at The Permanente Medical Group save more than 15,000 hours of paperwork in a year, giving them more valuable time to focus on patient care.
However, the real value comes when implementation balances efficiency, data security, and human oversight. AI should serve as an assistant—not a replacement—helping clinicians work smarter while ensuring safe, personalized care.
At Adamo Software, we help healthcare organizations build AI-powered solutions that are secure, flexible, and based on real-world clinical needs. If your group is exploring this path, our experts are ready to guide you every step of the way.





