EMR implementation: Challenges, solutions and costs breakdown

EMR implementation is an essential process for healthcare organizations to improve patient management. However, it still has a few challenges. Many healthcare facilities face the challenge of adapting to new technologies. Therefore, understanding this will prepare you to implement your EMR system effectively.
This article will identify several difficulties commonly encountered during EMR implementation. We will also highlight some of the practical recommendations for overcoming these challenges. Moreover, a detailed breakdown of the associated costs will also be included at the end for your reference.
I. What is EMR implementation?
EMR implementation is basically a change from paper-based charts or old systems used in hospitals or clinics to a new electronic system.
The process usually includes these steps:
- Planning beforehand
- Pick the right software
- Adapting it for the practice
- Training your personnel
- Performing the various tests and checking on the system
This last process is known as going live, during which everyone begins utilizing the new EMR software.
II. Step-by-step guide for a successful EMR implementation
1. Know your goals and objectives
What are your goals and objectives in implementing EMR? Make sure you decide on them before you begin the process. Ask yourself questions like, what do you hope to achieve with this new system? Understanding your goal will guide the process and help you know whether you’re progressing.
Here are some common goals for EMR implementation projects:
- Cost optimization: Minimize costs by eliminating as many opportunities as possible for people to do things manually and independently.
- Increase revenue: Increase revenue by attending to more clients.
- Maintain reimbursements: Always ensure to use certified EMR to enable you to receive payment from Medicaid/Medicare.
Concentrating on specific objectives lets you determine what features and equipment your EMR system should include to fulfill your requirements.
2. Choose the right people for your team
Teamwork is essential for successful EMR implementation. To get it right, you’ll need input from people from all over the department.
Here’s who you should involve:
- Healthcare staff or nurses: They know the workflows, so they will be able to shape the system according to their needs.
- Key stakeholders: Also include people from other critical areas like billing because they’ll also need to use the system.
- A project manager: Having someone in EMR projects who understands the process will keep things on track.
It also makes sense to have a separate team of experts, including developers, integration specialists, and testers. They’ll set up and customize the system to fit your practice.
Because EMR implementation is so complex, following expert advice and proven strategies will be the best way to ensure you get it right.
3. Set up a budget and timeline
Your first step here is to assign yourself a rough budget and time frame for your EMR implementation. It will be your guide, knowing how much you’re okay spending and what deadline you should set.
Using this top-down approach, you will know what to expect when comparing EMR options and getting vendor quotes.
4. Get together and define EMR requirements
It’s now time to brainstorm with your team. Determine the actual resources that would be required to run the EMR.
Some of the key areas to pay attention to include:
- Workflow processes
- User roles
- The requirements for hardware and network
- Complying with HIPAA
These requirements help you estimate the amount of work required to implement and also help you measure your team’s progress.
5. Make a shortlist of EMRs and run demos on them
Once you’ve done with the requirements, shortlist a few EMR systems that meet the requirements.
Run demos of these systems with your team and see if these systems suit your needs. Make sure they support critical workflows or are open to modification without too much disruption.
6. Decide on your best EMR option and implement it
Evaluate carefully to choose the EMR system that best suits the organization and then switch to implementation.
The project manager will oversee progress while your team sets up the system. Stakeholders can get involved for quick and required testing and feedback.
Using what you learn during that research, adjust your budget and timeline at this stage. Refinements might include:
- Payments for your team
- The EMR system’s cost
- Time needed for customization and testing
This will require a solid timeline. Staying on track with EMR implementation while including all the steps, from planning and data migration to testing and post-implementation evaluation.
7. Move your data
EMR implementation requires data migration, and it must be treated with special attention. This step is where the patient’s records, clinical data, billing information, and other documents are transferred to the new EMR system.
Any mistakes and missing data bring both clinical and administrative problems. Hence, careful planning and execution are needed to avoid mistakes. It is highly recommended that you have a data migration expert on your team. The goal is to have a smooth transition with no (or minimal) downtime, and your data remains intact and available.
8. Test the new EMR system
EMR implementation involves a crucial step of testing the new system, which often happens in two stages.
First of all, developers must make sure that the system being developed meets all requirements and has no technical bugs. They look at how EMR works and find things before users are exposed to it.
The system is then tested by super users, who are experienced providers who will use it every day. They’re these users who put the system through its pace hands-on, trying to understand how well it works with patient care workflows. Based on real-world scenarios, they offer insights into usability and efficiency.
Full access to all features gives super users the ability to check out all the features. Their expertise will help the EMR become both effective and easy to use for everyone.
9. Conduct comprehensive staff training
When testing is complete, your team has to be trained to use the new EMR system. This effort can be led by super users who use their knowledge to train colleagues. Staff might learn faster because it’s their firsthand experience with the system, and they feel more confident using the EMR.
10. Launch your EMR
It’s time to launch the EMR now. Clinics and hospitals can choose between two approaches: Gradual rollout or all-at-once deployment.
Pros and cons of each method exist, and your decision should fit in with your overall implementation strategy. A successful launch will depend on having a clear rollout plan that helps minimize disruptions.
11. Evaluate success metrics and user satisfaction
Once you’re living with your EMR system, you should monitor the performance metrics closely. These metrics might include:
- System uptime
- Speed of operation
- Ease of use
- Error rates
They all set out to boost productivity. The EMR should remove cumbersome tasks and not create new problems. It will help you to spot the areas where you can improve regularly by reviewing these metrics.
But that’s just half the story. It’s also important to evaluate user satisfaction. Ask yourself:
- Are providers comfortable with the system?
- Can patients easily access their health records?
- Is administrative work now more efficient?
Users’ feedback can also tell how well the system satisfied everyone’s needs. You can gather this input via surveys, our feedback forms, or even direct interviews. They will give you insights to fine-tune your EMR system even further.
You can explore more about What is EMR in Healthcare: Types, Features, Cost here.
III. Top 10 EMR implementation challenges
EMR implementation doesn’t have to be disruptive, but many practices have some tough challenges. Common obstacles during the process include the following.
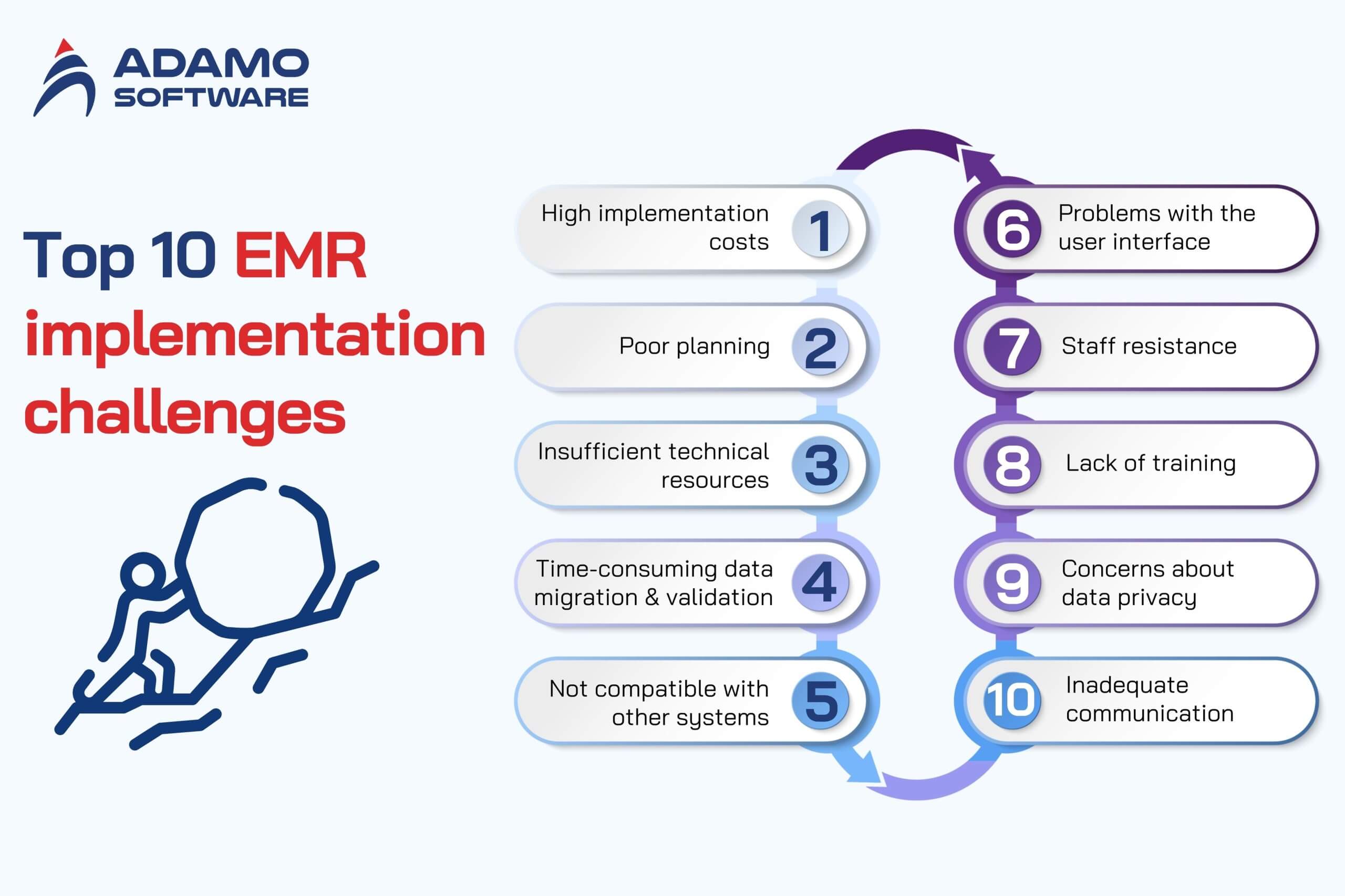
1. High implementation costs
The costs of EMR implementation are frequently a big hurdle for many practices, especially for the smaller ones. A survey indicates that the total cost of purchasing and installing the system per provider varies between $15,000 and $70,000. You may encounter additional unexpected costs, such as upgrades, equipment, and interface fees.
2. Poor planning
The main reason why many EMR implementations fail is poor planning. A successful plan requires detailed, thorough thought so you can carry it out in detail and with great care.
3. Insufficient technical resources
Many smaller practices don’t have in-house IT support, so it’s difficult to implement the EMR system. And there can be problems with not having the right hardware as well. That’s why choosing an experienced EMR provider can help with this challenge.
4. Time-consuming data migration and validation
Data migration and validation into another EMR system can be time-consuming and costly, regardless of whether you are switching from paper charts. However, the success of the system depends on keeping your data intact.
5. Not compatible with other systems
An EMR works smoothly only if it integrates with other systems. For instance, if your practice has an in-house lab, the EMR must be able to interface with the lab system to share accurate data. This can be a real issue unless integrated properly.
6. Problems with the user interface
EMR systems are not one size fits all. The more they fit into your practice’s workflow, the more usable they will be. When your system fits well, your staff and providers are more likely to embrace and assimilate the system.
7. Staff resistance
Resistance could be coming from all areas of your practice. Some staff may struggle with using computers, for instance. Other people might fear using the system will slow them down or make their jobs less efficient.
8. Lack of training
It’s hard to commit training time around a hectic practice. Some staff members who take time away from their regular duties might worry that they will lose business for physicians and management. However, skipping thorough training results in long-term inefficiencies.
9. Concerns about data privacy
Federal and state rules on privacy strictly guard health information, and violations come with hefty financial penalties. Selecting the right EMR system is not the only thing involved in protecting patient data. Last, it also concerns how your internal infrastructure protects information.
For hosted or cloud-based systems, you must know that your provider is HIPAA compliant, and your data is secure. If the data is not stored in your practice, you are still liable for protecting that data.
10. Inadequate communication
It is important to have strong communication throughout the implementation process. If staff aren’t aware of new changes, they may feel unprepared or uninterested, and that will undermine the system’s success.
IV. Tips to avoid common EMR project pitfalls

1. Underestimating the scale of change
EMR implementation is not a simple software project. It’s a gigantic change management effort. Almost everyone in the organization is impacted by an EMR system, changing workflows and decision-making processes.
There are multiple potential impact paths to streams and events, every configuration choice can affect upstream and downstream systems, processes, or workflows. Expecting these broad impacts can make staff already carrying a load bearing down, only aggravating them with frustration and resistance.
However, to avoid this, staff and clinicians should be engaged early in the process. Now’s the time to rethink how things get done and improve efficiency. This helps you minimize disruptions and minimize organizational risk by helping teams embrace the change.
2. Insufficient training
A major peril in EMR implementation is the lack of tailored training. Too many organizations don’t plan or deliver training in the context of real-world workflows, which results in lower adoption rates and frustrated users.
Training should ideally go beyond simple sessions. That should include one-on-one follow-ups and great ‘at-the-elbow’ support during go-live to address the untold concerns of the day. Unfortunately, too many organizations today rely on virtual training so heavily that it’s optional, further detracting from user readiness.
Training is mandatory, and users won’t be able to use the system without proper training. In addition, thought needs to be given to how staff can be covered during training. This would be useful if there were enough trainers and if various training schedules could be offered to suit shift work. A mix of in-person and virtual options can meet the varying needs of clinicians and staff, improving both engagement and outcomes.
3. Misjudging the technology and data uplift
The most common mistake is underestimating the data and technical challenges accompanying EMR implementation. Many new EMR systems, however, need to connect with numerous internal and external legacy systems. Poor data sharing in the EMR can severely curtail the value of the EMR and its transformational potential.
Typically, organizations are trying to “lift and shift” their existing reports into the new EMR, assuming minimal changes. However, as workflows need to be changed, so do the legacy reports and the data architecture that sustains them. A modern EMR is a single source of truth, allowing one to streamline reports and recast key performance metrics.
Data governance policies with strong data quality and integrity should be established. These are the building blocks of advanced analytics and underpin the new EMR system to deliver informed decision-making and the innovation to follow.
4. Thinking in silos
EMR implementation as a sequence of isolated departmental projects could result in major problems. This can result in broken processes, which in turn slow patient care and lower its quality.
Instead, the EMR project should be seen as an opportunity to improve the flow between workflows and across the enterprise. Visualize the full patient journey and seamless information sharing across staff, clinicians, applications, departments, and, in some cases, even with external partners.
The holistic customer-focused perspective will streamline operations and maximize the system’s value.
V. How long does it take to implement EMR?
There is no standard timeline for EMR implementation because many factors influence how long it will take to put one in place. The process is so complicated that many variables can either shorten or lengthen it. So, it is based on the setting and the particular product being implemented.
Due to these variables, we can’t say there’s a one-size-fits-all timeline for EMR implementation. However, experts involved in the process can estimate accurately to reduce uncertainty. Working on the project with experts will let you know more or less how long it will take and let you plan accordingly.
VI. EMR implementation costs breakdown
When implementing an EMR system, the costs are typically divided into three categories. They are initial setup costs, ongoing operational costs, and indirect costs.
1. Initial costs
These are the one-time expenses that occur at the beginning of the implementation:
- Software licensing fees: The amount needed to be paid for the purchase or subscription of the EMR software.
- Customization costs: The cost of adjusting the system to the practice’s needs.
- Hardware costs: Servers, storage, workstations, computers, tablets, and network infrastructure such as routers and switches are included in this type of cost.
- Implementation services: Fees for planning, implementing, and configuring the system, as well as installation and configuration.
- Training and support costs: Costs of staff training for the new system and ongoing support.
- Data migration costs: Transfer of data from the old system to the new one.
2. Ongoing costs
These are recurring expenses that continue after the initial setup:
- Subscription fees: Are generally associated with cloud-based EMR systems and include coverage for software updates and technical support.
- Ongoing maintenance and support costs: Include regular software updates and continuous technical support.
- Hardware maintenance: Costs for upgrades and replacing hardware components over time.
For a small to medium-sized practice in the U.S, ongoing operational costs per user per year are estimated to be between $4,000 and $24,400. The more the practice, the more the cost.
3. Indirect costs
These costs are not always obvious but can add up over time:
- Productivity Losses: The learning curve on the new system and the possibility of employing some temporary staff while the transition is made.
- Compliance and Security Costs: Protecting patient data and ensuring that (for example, HIPAA and GDPR) the system meets healthcare regulations.
On average, the total cost of ownership for the first year is $16,400-$68,400 per provider.
VII. How Adamo Software is your ideal partner for successful EMR implementation

If you’d like to have successful EMR implementation in healthcare, Adamo Software is your ideal partner. Our team of experienced IT experts understands clearly the hurdles of EMR implementation. Hence, we offer tailored healthcare solutions available to meet your specific operational needs, as well as your compliance standards.
Adam offers a disruption-free tool to ensure seamless migration, data migration, and interoperability with existing systems. We help maintain staff adoption by focusing on user-friendly interfaces. Security, as well as compliance, is a high priority for us, and you will see that your EMR system conforms to HIPAA regulations. As such, we also provide support and maintenance to help your system continue to run smoothly on a regular basis.
When working with Adamo, you have a reliable partner who will work with you to make the most of your EMR implementation. Contact us to begin your journey to the effective management of your health care!