Electronic Data Interchange (EDI) in healthcare: What is it? How to implement it?

Electronic Data Interchange is a hot topic. The CAQH Index Report indicates that healthcare industry can save $20 billion by completely electronic transactions.
Every day, healthcare organizations deal with vast quantities of data, including patient records, claims, lab results, and prescriptions. Nevertheless, not all data are equal. Different systems and formats can make data exchange challenging, expensive, and prone to error.
Approximately 50% of hospitals in the United States believe that the growing volume of unstructured data will be the greatest barrier to enhancing healthcare interoperability, thereby undermining connected care initiatives. Healthcare EDI transactions are a dependable solution that can help hospitals surmount these obstacles.
I. What is EDI in healthcare?
Electronic Data Interchange (EDI) in healthcare is a secure method for transmitting data between healthcare institutions, insurers, and patients, using standardized message formats and protocols.
The introduction of Electronic Data Interchange dates back to the 1960s, when there were more than 400 different standards in use. At that time, conversion errors, poor interoperability, high IT costs, and security vulnerabilities were common issues. The implementation of EDI solved these issues by facilitating the transmission and interpretation of data.
The HIPAA EDI Rule requires covered entities (i.e., health plans, clearinghouses, and care providers) that electronically transmit medical information to use uniform standards for all healthcare EDI transactions. HIPAA Electronic Data Interchange compliance requires the use of ASC X12 protocol when transmitting HIPAA documents (i.e., any documents containing health-sensitive data)
The ASC X12 protocol ensures the security and veracity of medical data by being the only acceptable format for HIPAA EDI transactions. It mandates that all parties involved in the transmission adhere to particular data specifications. In particular, the information is converted into computer (non-human) language before being transmitted to a receiving computer. Also, standard codes are assigned to all documentation sets.
Organizations utilize HIPAA Electronic Data Interchange software solutions to generate standardized EDI documents and convert them to common business formats.
II. How does EDI work in healthcare?
Typical healthcare EDI transactions involve 5 stages. Let’s use a medical provider’s inquiry to a payer as an example.
1. The medical provider initiates the inquiry by providing specific information, such as the member identification number and date of birth.
2. The inquiry goes to a clearinghouse that the provider has contracted.
3. The clearinghouse transmits the inquiry to the payer.
4. The payer responds to the clearinghouse.
5. The clearinghouse transmits the response to the medical provider.
All parties transmit the data using ANSI ASC X12 codes, the standard that regulates all EDI transaction codes, including those for electronic healthcare transactions.
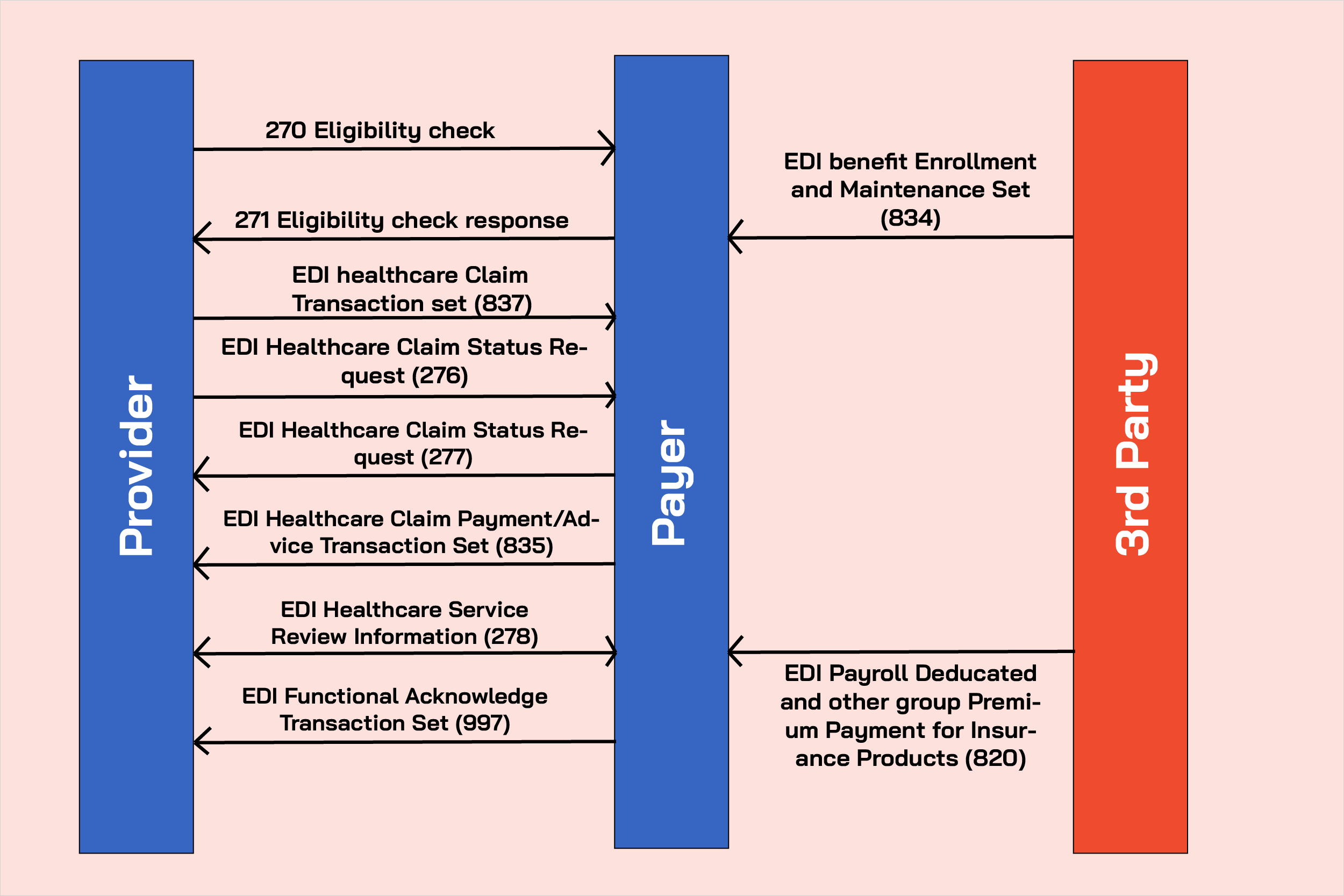
III. What are healthcare EDI transaction types?
1. Healthcare claim transaction (836)
Healthcare organizations utilize EDI 836 for the submission of healthcare claim billing information, encounter data, or both.
This transaction does not apply to retail pharmacy claims. Typically, healthcare providers send these to payers. This occurs either directly or through billers and claims clearinghouse serving as intermediaries.
2. Retail pharmacy claim transaction
Healthcare professionals and regulatory agencies can submit retail pharmacy claims via claim transactions. This type of EDI healthcare transaction allows different entities to send claims for retail pharmacy services and billing payment information to payers.
3. Healthcare claim payment/ advice transaction (835)
Insurers use it to make payments and send Explanation of Benefits (EOB) remittance advice to healthcare providers.
4. Benefits enrollment and maintenance set (834)
Employers, unions, government agencies, insurance companies, associations, and healthcare organizations pay claims using transaction 834. The objective of this form of translation is to enroll members in a healthcare benefit plan.
5. Payroll deducted and other group premium payment for insurance products (820)
Transaction 820 facilitates the payment of insurance premiums. Financial institutions receive information from healthcare institutions via these transactions.
6. Healthcare Eligibility/ Benefit Inquiry (270)
This transaction set is used by healthcare institutions to transmit inquiries to financial institutions and government agencies regarding healthcare benefits and subscriber eligibility.
7. Healthcare Eligibility/ Benefit Response (271)
Its primary function is to respond to requests for information regarding the healthcare benefits and eligibility of a subscriber or dependent. Similar to the previous transaction, healthcare institutions use this one to transmit data to financial institutions and government agencies.
8. Healthcare claim status request (276)
This transaction is utilized by healthcare providers to request or confirm the status of previously submitted healthcare claims to a payer, such as an insurance company.
9. Healthcare claim status notification (277)
Providers can use Transaction 277 to report on the status of previously submitted claims. This form of transaction is utilized by healthcare payers and insurance providers.
10. Healthcare service review information (278)
To request authorization from a payer, such as an insurance company, hospitals use transaction 278.
IV. Importance of EDI
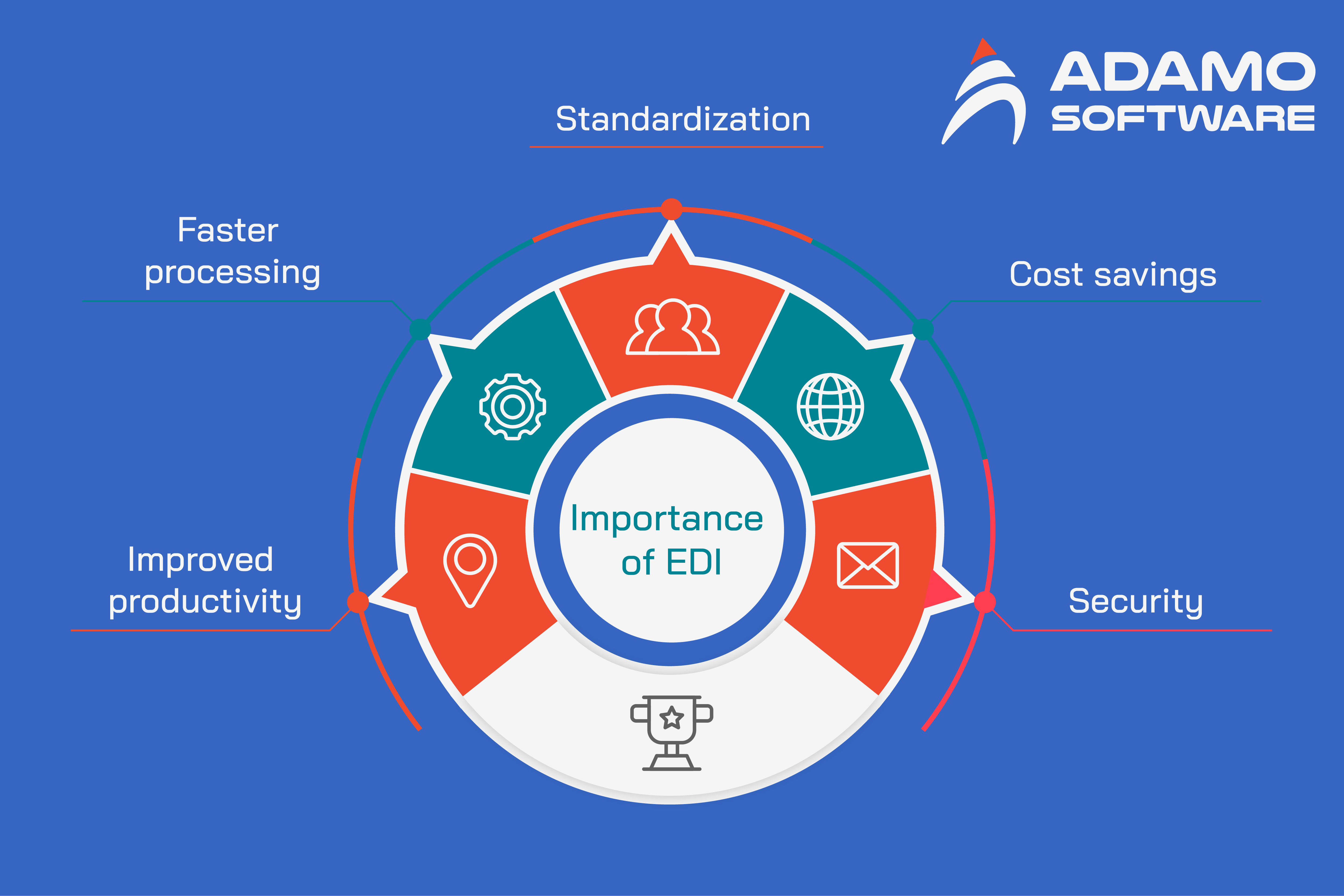
1. Standardization
Using Electronic Data Interchange, HIPAA aims to establish national and global standards for electronic healthcare transactions. HIPAA EDI transactions facilitate the exchange of healthcare data that is compliant, accurate, and efficient. HIPAA EDI standards are not, however, limited to patient transactions or health information transmission. It also includes standards for employees’ compensation in healthcare.
2. Cost savings
Because it helps eliminate paper trails and digitize all transactions, enabling EDI healthcare transactions can result in reduced handling costs for processing healthcare documents. With EDI, healthcare organizations can generate significant cost savings: $1 per claim for health plans, $1.49 for physicians, $0.86 for others (WEDI estimates).
3. Security
Healthcare EDI systems permit the transmission of information between healthcare providers and payers of insurers in a secure manner. As mandated by HIPAA regulations, EDI now facilitates secure data transmission for these healthcare transactions. EDI transactions in healthcare can be restricted to authorized users, facilitating the secure administration and access of healthcare data.
4. Improved productivity
Utilizing EDI for healthcare transactions increases productivity by enabling a high level of precision, efficiency, and speed. Due to the limited human intervention, fewer errors occur. EDI reduces the occurrence of manual data errors, shipping errors, incorrect invoicing addresses, and other similar errors. Due to the use of electronic attachments, which streamlines the process, EDI has proven to be an efficient instrument for insurance claims documentation.
With the use of EDI, healthcare providers and payers have experienced fewer denials and requests for revisions. Additionally, transactions with multiple customers can occur simultaneously. As a consequence, healthcare stakeholders can now concentrate on more pressing matters.
5. Faster processing
Electronic Data Interchange benefits not only healthcare professionals and institutions, but patients as well. One of the significant outcomes of HIPAA was the right of patients to access their health information, which was “crucial to reinventing the healthcare delivery system.” EDI transactions are advantageous for patients because they accelerate the claims and benefits procedure.
V. Impact of healthcare EDI
1. Accountable Care Organization (ACO)
Through a network of collaborating providers, the Accountable Care Organization (ACO) model focuses on enhancing care coordination, increasing patient outcomes, and reducing healthcare costs.
For instance, when a patient requires a referral to a specialist, the primary care physician can use EDI transaction sets such as the Continuity of Care Document (CCD) or Healthcare Services Review (EDI 278) to electronically transmit pertinent patient information to the specialist. These transaction sets guarantee the transfer of comprehensive information, thereby facilitating personalized care and enhanced outcomes.
In the ACO model, EDI also serves a crucial role in care coordination. Health Care Claim (837) and Eligibility Inquiry (270) transaction sets facilitate the exchange of claims information and eligibility verification, respectively. Electronic submission and processing of claims by providers reduces administrative burdens and improves ACO-wide efficiency.
EDI also facilitates population health management within ACOs. Health Care Claim (837) and Health Risk Assessment (HRA) transaction sets facilitate the secure exchange of population data, such as demographic information and disease registries.
This data-driven approach enables providers to identify populations at risk, implement preventative measures, and manage chronic conditions proactively. Through the utilization of EDI transaction sets in population health management, providers can improve outcomes and reduce costs.
2. Patient-Centered Medical Home (PCMH)
Through a team-based approach, the Patient-Centered Medical Home (PCMH) model emphasizes comprehensive, coordinated, and patient-centered care. It focuses on enhancing the patient experience, enhancing care quality and outcomes, and decreasing healthcare expenditures.
Using EDI transaction sets such as the Continuity of Care Document (CCD), Electronic Lab Result Reporting (ELR), and Referral Authorization (278I), for instance, healthcare providers within the PCMH can share vital information efficiently. Consider a scenario in which a patient with chronic conditions consults a primary care physician.
The healthcare provider must consult with a specialist and refer the patient for additional evaluation. Using EDI, the primary care provider electronically transmits the referral information to the specialist, including the patient’s medical history, medications, and the reason for the referral. This guarantees that the specialist has the essential context for specialized care.
The specialist can then use EDI to submit the consultation report and recommendations back to the primary care provider, seamlessly integrating patient information. This allows the primary care provider to review and coordinate the patient’s next care actions.
3. Specialist Hospitals and Population-Specific Care Units
Specialist Hospitals and Population-Specific Care Units are specialized healthcare facilities that enhance patient outcomes and experiences for specific medical conditions or populations.
However, coordinating with primary care providers and effectively allocating resources pose obstacles to the implementation of this model. EDI overcomes these obstacles by facilitating the exchange of patient data, diagnostic reports, and treatment plans.
In addition, EDI facilitates ongoing collaboration and communication between specialized institutions and referring providers. Health Care Claim Status Request (276/277) facilitates the electronic exchange of patient status updates, test results, and treatment modifications. Coordination and communication facilitated by EDI ultimately result in better patient outcomes in specialist hospitals and populations.
VI. How to make EDI
1. Building a proper system architecture
Create a robust system architecture or enhance the current one in order to:
– Permit users to efficiently manage (store, generate, modify, retrieve, and save) EDI data.
– Implement a secondary system and resilience scenarios to guarantee business continuity.
– Ensure prompt responses to requests and transaction completion.
2. Using role-based access
Access control is essential to the security of your healthcare application. To prevent unauthorized data access, it is imperative to classify users into distinct groups and categories (administrators, care providers, patients, etc.) and assign them role-based permissions.
3. Using encrypted communication
According to the latest Centers for Medicare & Medicaid Services (CMS) standards, all providers must use and maintain systems/platforms that are secure, encrypted, and minimize the risks to patient privacy and confidentiality. Encryption is crucial for securing communication channels and infrastructure and ensuring that cybercriminals cannot read the exchanged information, even if they intercept it.
4. Keeping PHI safe
Protected health information, be it a health record or payment for healthcare services, is a fundamental element of any healthcare system. You can address it by employing:
– Smart keys, biometrics, secure user IDs, and PINs for hack-proof and secure user identification systems
– Procedures for emergency access, automatic sign-off, security alerts, and data restoration
Developing EDI compliance is no simple task. Implementing document generation (EDI mapping and translation), testing, validation, and transfer algorithms requires extensive knowledge and skill. Consequently, it is essential to discover a reliable partner in order to meet all of these requirements.
You can explore more about What is Health Data Management: Benefits, Challenges and HDM Software here.
VII. Regulation of HIPAA drives EDI in healthcare & EDI Standards
1. HIPAA regulation is driving healthcare EDI
HIPAA is a federal law issued by the Department of Health and Human Services (HHS) that protects patient privacy. The Health Insurance Portability and Accountability Act (HIPAA) of 1996 came into effect to facilitate the exchange of healthcare documents.
HIPAA required the HHS to implement regulations to protect the privacy and security of healthcare information to accomplish this. The Department of Health and Human Services (HHS) enacted two rules governing the establishment of EDI standards. The HIPAA Privacy Rule and HIPAA Security Rule have been released.
“The Privacy Rule, also known as the Standards for Privacy of Individually Identifiable Health Information, establishes national protection standards for specific health information. The Security Standards for the Protection of Electronic Protected Health Information (the Security Rule) establishes a national set of security standards for the protection of certain health information held or transferred in electronic format.”
Before HIPAA, the healthcare industry was disorganized and used over 400 paper forms to exchange documents. Data administration of healthcare documents was manual, time-consuming, and rife with errors, which raised significant concerns for patient information and data security.
Post-HIPAA, the American National Standards Institute (ANSI) or American National Standards Committee (ANSI) developed the ASC X12 standard for transmitting healthcare data.Typically, HIPAA EDI standards govern the transmission of documents among healthcare providers, insurance companies, patients, healthcare clearinghouses, and business partners.
2. Healthcare EDI standards for uses
VIII. Adamo Helps You Comply with EDI in Your Healthcare Software Solutions
Integrating healthcare EDI is a challenging task that needs a high level of programming skills and tactics of HIPAA standards. Our Adamo development team will help you build a custom application that performs various functions and avoids a case of HIPAA violations.
Building successfully and completing a wide range of healthcare software development projects, Adamo can become your IT trusted healthcare software development partner in the area. Our experts consult you on implementing EDI, build bespoke healthcare solutions and fine-turn your existing software, thus it complies with various regulatory requirements like HIPAA. Contact us now, and we will help you execute HIPAA EDI integration and more.